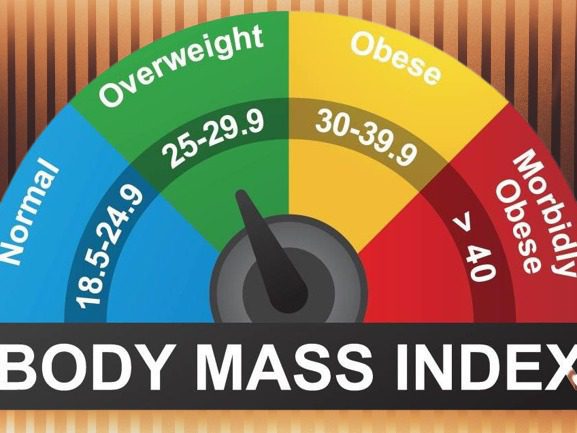
Rethinking BMI: Body mass index (BMI) has long been used as a measure to determine whether an individual’s weight falls within a healthy range. However, a recent study challenges the notion that BMI alone is a reliable indicator of a person’s health. This article explores the findings of the study, highlights the limitations of BMI as a health indicator, and discusses the need for alternative measures to assess an individual’s overall well-being.
The Study Unveils Surprising Findings
In a study published in PLOS One, researchers analyzed data from over 550,000 U.S. adults over a nine-year period to examine the relationship between BMI and mortality risk. The results revealed something unexpectedolder adults (65+) with BMIs between 22.5 and 34.9, as well as younger adults with BMIs between 22.5 and 27.4, showed no significant increase in mortality risk. This challenges the commonly held belief that a higher BMI automatically corresponds to a higher risk of death.
The Limitations of BMI as a Health Indicator
For decades, BMI has been widely used to categorize individuals as underweight, normal weight, overweight, or obese based on their height and weight. However, health care professionals have criticized this approach, emphasizing that BMI fails to account for important factors such as body fat percentage, variations in disease risk among different races and genders, and overall body composition.
Shifting Paradigms
New Guidelines for Health Assessment: Recognizing the limitations of BMI, the American Medical Association has recommended using additional measures to assess a person’s health. These include evaluating waist circumference, fat distribution, and genetic factors. By considering these additional factors, healthcare providers can gain a more comprehensive understanding of an individual’s overall health status.
Waist Circumference as a Strong Indicator
The study findings indicate that waist circumference may be a stronger indicator of health than BMI alone. When individuals with equal BMIs but different waist circumferences were compared, those with larger waist circumferences were associated with a higher risk of death overall. This highlights the importance of considering not only weight but also where fat is distributed in the body.
Examining Specific BMI Ranges and Mortality Risk
While the study revealed no significant increase in mortality risk for individuals within certain BMI ranges, it did confirm that a BMI of 30 or more is still associated with a greater risk of death. Additionally, younger adults with BMIs between 27.5 and 29.9 faced a nearly 20% higher risk. These findings emphasize that while BMI may not be the sole determinant of health, extreme values should still be taken into consideration.
Also Read: Philadelphia Shooting
Challenging the Notion of BMI as a Measure of Health
Dr. Fatima Stanford, an obesity medicine specialist, points out that relying solely on BMI equates leanness with health, disregarding other important factors. For instance, individuals with substance abuse disorders, tobacco use, or disordered eating may have a lean physique but may not be healthy. It is essential to move beyond BMI and consider a broader range of health indicators.
BMI and its Complicated Relationship with Weight-Related Disease
Previous research has highlighted the issues with using BMI as a measure of obesity and weight-related diseases. Studies have shown that nearly half of the participants considered overweight and a significant percentage of those considered obese were metabolically healthy. Similarly, individuals with “normal” BMIs may still exhibit signs of obesity-related health complications.
Racial and Ethnic Considerations in BMI Assessment: Another aspect that complicates the use of BMI as a health indicator is its limited applicability across different racial and ethnic groups. BMI thresholds may not account for the specific risks faced by certain populations. For example, Asian individuals may experience metabolic diseases at lower BMIs,while Black women may have different health outcomes at higher BMIs. Recognizing these differences is crucial to avoid misclassifying individuals and overlooking their unique health needs.
The Importance of Updated Data Sets: The study authors noted that past research on BMI and mortality risk predominantly included data from the 1960s to 1990s, with mostly white participants. Given the changing demographics of the United States, relying solely on these outdated data sets may not accurately represent the current population. The study addressed this concern by including a diverse participant pool, representing a range of racial and ethnic backgrounds.
Beyond Mortality Risk
Additional Health Considerations: Critics of the study argue that focusing solely on mortality risk overlooks the broader health implications of higher BMIs. Conditions such as Type 2 diabetes, high blood pressure, cholesterol abnormalities, and various types of cancer are associated with elevated BMI. It is essential to consider these additional health risks when evaluating an individual’s well-being.
According to the Centers for Disease Control and Prevention (CDC), individuals with BMIs of 25 or higher face an increased risk of developing various health conditions. These include high blood pressure, high cholesterol, Type 2 diabetes, and certain types of cancer. While BMI is a useful screening tool, it should not be the sole determinant of an individual’s health status.
Future Measures of Obesity Assessment
As healthcare professionals strive for more accurate measures of obesity, the study’s authors and experts alike advocate for incorporating additional factors such as body fat percentage. BMI alone fails to capture the full complexity of an individual’s body composition and its impact on health. By considering multiple indicators, clinicians can gain a more nuanced understanding of a person’s overall well-being.
Conclusion of Rethinking BMI
The recent study challenges the long-standing belief that BMI alone is a reliable indicator of a person’s health. While BMI can provide a general assessment, it should not be the sole determinant of an individual’s well-being. Incorporating additional measures, such as waist circumference, body fat percentage, and genetic factors, can provide a more comprehensive understanding of an individual’s health risks and needs. It is essential to move beyond the limitations of BMI and embrace a more holistic approach to assessing and promoting overall health.
Our Reader’s Queries
Why is BMI not used anymore?
The AMA has recently implemented a new policy, acknowledging the problematic nature of using BMI as a measurement. This is due to its negative historical impact, its role in excluding people of different races, and its reliance on data from previous non-Hispanic white generations.
What is replacing BMI?
A recent study suggests that waist-to-hip ratio could be more effective than body mass index (BMI) for managing weight. The research, featured in JAMA Network Open, reveals that waist-to-hip ratio may provide better insight into health risks and medical treatments.
Why is BMI misleading?
A major factor is that someone with high muscle mass and low body fat can register the same BMI as someone with obesity but less muscle. Additionally, BMI fluctuates depending on a person’s age and activity levels, since body fat percentage varies. This inconsistency can lead to misleading results in certain scenarios.
What are the inconsistencies of BMI?
The BMI, calculated using a person’s height and weight, is an unreliable indicator of body fat and overlooks factors like muscle mass, bone density, body composition, and variations in race and gender, according to experts at the Perelman School of Medicine, University of Pennsylvania.